TUESDAY, 21 JULY 2015
Glial cells, or glia, are essential for the brain and nervous system to work properly. Here at Bluesci Neuroscience, we really like glia: a few months ago, we covered the controversial study that created a mouse with its entire glial cell population derived from humans. This time, a paper published last month in Nature Neuroscience has revealed more about the maturation and maintenance of these cells – which, surprisingly, requires bacteria.The specific glial cells in question are microglia, the immune defence cells of the brain. Microglia are found behind the protective blood-brain barrier, which separates the brain environment from the rest of the body, where they scavenge and remove cells and debris that might be harmful to the brain. They are also important in early nervous system development and maintaining connections between nerve cells in the brain during adulthood. Since they have a central role in brain function, it isn’t surprising that genes associated with microglia are now being implicated in neurological disorders (such as Alzheimer’s) and mental illness.
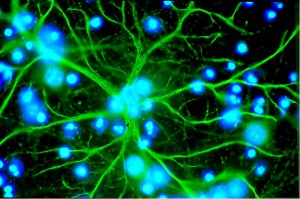
Glial cells have complex morphologies and form many connections with other cells in the brain.
Given that microglia are secluded behind the blood-brain barrier, it seems strange that bacteria – which the barrier usually keeps out of the brain – would be important for their development and function. However, it’s true that many bacteria in the body are actually beneficial, for example the large collection of bacteria in the gut, which help us digest food properly. In fact, gut bacteria are linked to both nervous system function (for instance, by modulating the hormonal control of stress responses) and immune function (by regulating the gut immune response during infection). Until now, though, no-one had studied the connection between beneficial bacteria and the immune cells of the brain.
Daniel Erny and colleagues set out to answer this question by studying microglia function in ‘germ-free’ mice, which had been raised in a sterile environment. The researchers found that microglia in the germ-free mice were abnormal: they didn’t switch on the right genes, their shape was different from microglia in healthy control mice, and they appeared ‘immature’ even in the adult brain. They also mounted a weaker than normal immune response to toxins and pathogens introduced into the brain.

Germ-free mice are a useful model for the role of bacteria in normal body function
Germ-free mice grow to adulthood without ever coming into contact with microbes, so these microglia defects could just be a developmental problem. However, when Erny et al. treated normal mice (i.e. mice that had grown up with healthy bacterial populations) with antibiotics, which kill most gut bacteria, they observed exactly the same defects. When these mice were taken off antibiotics and re-exposed to beneficial bacteria, their microglia promptly recovered – showing that even removing the normal bacterial population from adult mice was enough to cause microglial defects.
Gut bacteria seem to be the important players here, too. When both germ-free and antibiotic mice were given short-chain fatty acids (SCFAs), which are small molecules produced by bacteria in the intestine, the microglial defects were again reversed. SCFAs have also been implicated in immune function in the rest of the body, and they can easily pass into the bloodstream from the gut. They are also small enough to be selectively transported across the blood brain barrier, so they’re likely to be at least one of the signals between bacteria and the brain.
These results could help point us towards potential treatments of neuroinflammatory and microglia-mediated disorders, though more work needs to be done on how exactly SCFAs ‘push’ defective microglia back into normality. The take-home message for now seems to be: Take care of your gut – your microglia will thank you.
Further reading
Original paper: Erny et al. (2015) Nature Neuroscience 18, p. 965 (available here: http://www.nature.com/neuro/journal/v18/n7/full/nn.4030.html)
SCFAs and immunity: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3257741/ and www.pnas.org/content/111/6/2247.full.pdf
