MONDAY, 3 MAY 2010
The existence of the placebo effect is well established. The necessity of double blind, randomised trials with control groups shows how seriously the scientific community takes the influence of placebo on study results. However, the placebo effect is still poorly understood. Where does it come from? Why does it exist? Can and should we use it?Perhaps the last of these questions is the most controversial in current public health policy. The use of homeopathy by the NHS continues to fuel intense debate. Controlled studies suggest that it is the placebo effect that causes patients to see results from these alternative therapies. Is it unethical to frame these treatments as ‘medicine’? Furthermore, are scientifically developed drugs being turned down by patients when these placebos are administered? Is this safe?
Despite these concerns, the potential benefits of placebo therapies are thought-provoking. The effect has been reported to cause remission in a wide range of conditions: cancer, Parkinson’s, depression, and inflammatory disorders, to name a few. Probably the most commonly documented role of placebos is in providing effective pain relief, exemplified by accounts of soldiers injured in battle who feel no pain until they are in a place of safety. If physiological mechanisms underlie the observed placebo effect in pain relief, why shouldn’t we try to understand them and use them to our advantage?
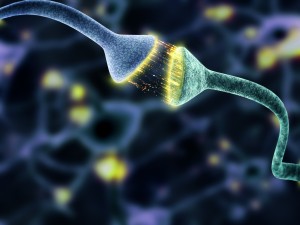
The argument that the placebo effect ‘is all in the mind’ is essentially true, but its apparent psychological activation does not imply the lack of a genuine mechanism. In the example of pain, it has been shown that descending neural systems from the midbrain are capable of modulating perception of pain by interacting with neuronal synapses in the spinal cord. These systems arise mainly from a part of the midbrain called the periaqueductal grey region (PAG) and a second area in the brain called the raphé nuclei.
Neurons extend from these areas down into the spinal cord to interact with the pain-carrying nerves arriving from the rest of the body. When the descending neurons in the spinal cord are activated they cause the release of a set of messenger proteins called enkephalins. Enkephalins are a type of opioid, naturally occurring pain relievers produced by the body’s nervous system. Each pain-sensing nerve has opioid receptors and when enkephalins bind to these receptors they inhibit the nerve’s ability to communicate its message any further. As a result, the brain can limit the number of pain signals that get through to the central nervous system, modulating our perception of pain. Pain-relieving drugs such as morphine work by targeting these same opioid receptors on pain nerves. Essentially, the brain is able to naturally relieve pain and the placebo effect is the psychological activation of this ability.
The effect is surprisingly strong. It has been shown that direct electrical stimulation of the PAG region is capable of inducing sufficient analgesia to enable abdominal surgery without anaesthetic. Interestingly, this effect is lost following intravenous injection of the drug naloxone, which binds to the opioid receptors and blocks them. Naloxone is normally used to counter the effects of overdoses of opiates such as morphine and heroin, which could lead to life-threatening inhibition of the central nervous system and respiratory system.
A recent study illustrates this principle in action. Volunteers were injected with capsaicin in their hands and feet, just under the skin. Capsaicin (the active ingredient in chilli peppers) is a potent stimulator of heat and pain receptors. When a non-medicated topical cream was applied to the site of injection, with the volunteers being told it was pain-relieving, they reported significantly less pain. Importantly, the analgesic effect was specific to the site at which the cream was applied and volunteers did not report any soothing effect at other untreated sites where capsaicin was also injected. The intravenous injection of naloxone again removed the pain-relieving effect.
This suggests that the placebo effect is not only significant but also site-specific. Studies in rats have shown that direct electrical stimulation of different parts of the PAG area induce site specific analgesia. This implies a neuronal mechanism within the brain that is able to modulate pain perception in particular parts of the body, and contrary to previous belief, a general release of opioids throughout the central nervous system does not underlie the effect. Naloxone’s blockage of the placebo effect on pain strongly suggests this is the same system being activated by higher centres in the brain when analgesia is expected. No other systems capable of achieving the same effect have been found. It seems that a complex system causes the placebo effect, including neurological circuitry within the brain that inhibits pain at specific sites upon belief that analgesia will occur.
Perhaps medical practitioners can take advantage of the placebo effect by initiating its activity, allowing them to alleviate pain in a site-specific manner. Given that unwanted and potentially dangerous side effects are potential consequences of many pain-relieving drugs, this would certainly be an attractive option. Moreover, it seems possible to activate it entirely psychologically and avoid off-target stimulation or inhibition of other nervous system components (the cause of side effects in conventional therapies).
Clinical use of the placebo effect is not without problems. The effect observed varies greatly between individuals, and the ethical implications of administering a ‘drug’ that contains no pharmacologically active ingredients are numerous. Also, as the activation of the placebo effect is psychological, its effectiveness might be reduced if the population being treated was made aware of the mechanism. More importantly, would a greater awareness of the placebo effect amongst the general population undermine the efficacy of current drugs since some of their success could be undocumented results of this phenomenon?
Whatever one’s views on the deliberate use of the placebo effect in pain medicine, a physical, neurological basis for it does exist. It may be only a matter of time before we also uncover the mechanisms behind the placebo effect in other conditions. As our understanding of the placebo effect is constantly improving, perhaps we should not be too quick to dismiss it as a valid potential treatment.
Ryan Breslin is a second year preclinical medical student