WEDNESDAY, 18 JANUARY 2012
We all have a good idea of how ageing affects our bodies. But how much do we know about the underlying reasons for these changes?As we grow old, our bodies become increasingly unable to function normally. Typical features of advancing years are often accompanied by diminished ability to recover from illness and injury. Many characteristic age-related changes in our bodies are linked to deterioration in tissue function, especially in what is known as the regenerative potential of tissues. The symptoms of this decline can range from serious problems such as atherosclerosis, osteoporosis and a weakening of the immune response to more superficial signs of ageing like wrinkles. The prevalence of many diseases such as cancer also increases dramatically with age.
To understand the science of ageing we have to get to grips with three features of the cells that comprise our tissues: their tendency to accrue damage, the consequences of the failure to repair this damage and the inherent limit in the number of times they can divide.
Damage accumulates over the lifetime of a cell. One scientific theory of ageing links the build-up of cellular damage to the mitochondria—compartments within the cell where molecules derived from food are converted into a form of cellular energy. Some of the unfortunate by-products of this process are molecules known as reactive oxygen species (ROS), which carry unpaired electrons and so are highly chemically reactive. One theory of ageing is based on the idea that ROS are responsible for inflicting damage on the DNA and proteins in the cell.
The cell uses several enzymes to mop up ROS, but these defence mechanisms are not perfect and are believed to deteriorate with age. Evidence in support of the theory comes from genetically modified mice. Mice which lack the genes for these protective enzymes have a significantly reduced life expectancy. However, findings in the nematode worm C. elegans have shown that loss of one type of protective enzyme actually extends (or at least does not reduce) lifespan. Although appearing contradictory at first, it is believed these results indicate that loss of the enzyme may alter mitochondrial function, outweighing the increased susceptibility of the cell to ROS damage. The study highlights the fact we still have gaps in our knowledge of a very complex field. It seems ROS are likely to play a role in ageing, but they are by no means the whole story.
Cellular damage is also caused by exposure to UV light and mutation-causing chemicals that can result in damage to DNA in the cell nucleus. This damage occurs through breaks in the double strands of the DNA helix and in changes to the individual bases making up the DNA comprising the genetic code. DNA encodes the proteins that are required for the cell to function properly, so damage here can have disastrous consequences.
The cell is able to monitor DNA damage through the p53 protein. p53 is able to initiate several responses depending on the severity of the damage. In the event of a catastrophe where damage leaves the DNA beyond repair, p53 can execute the cascade of biochemical events eventually leading to the death of the cell. This is the cellular equivalent of pushing the self-destruct button.
Extensively damaged DNA can lead to abnormal proteins being produced, which in some circumstances could allow the cell to divide uncontrollably, causing cancer. Therefore, the role of p53 is of such paramount importance that it has earned itself the nickname “guardian of genome”. p53 is often found to be mutated and unable to work properly in a high proportion of human cancers. In mice genetically engineered to have hyperactive p53, accelerated ageing is observed but cancer incidence drops. There is seemingly a fine balance between the anti-cancer effects of molecules such as p53 and the increased ageing that they may cause.
Another answer to the mystery of ageing may lie within the enigmatic entities known as stem cells. Most cells have an inherent limit on the number of times they can divide. Stem cells are different and are able to replace themselves through a process of self-renewal. This can occur symmetrically (where two identical daughter stem cells are produced), or asymmetrically. Asymmetric self-renewal occurs when one stem cell is produced alongside another cell that has begun the journey along a pathway of differentiation. In other words, the cell starts to get more and more specialised, eventually becoming totally specialised in order to fulfil a particular role, from the long, fat-insulated cells of the nervous system to the white blood cells of the immune system. Stem cells are therefore vital for the replacement of cells that are unable to divide themselves.
The capacity of our bodies to replenish tissues during our lifespan depends on a reservoir of tissue-specific stem cells. Researchers have proposed that the physiological decline in many organs with age could result from stem cell ageing. Ageing of the haematopoietic stem cells that give rise to all blood cell types is associated with a less effective immune system, as the white blood cells that guard us from pathogens are reduced in number. Similarly, in the brain, the decrease in the production of new neurons is linked to a reduction in the number of neural stem cells.
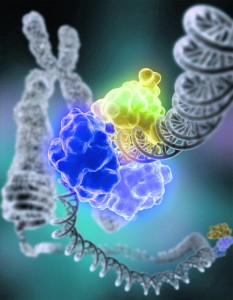
But why should stem cells age? Apart from the gradual accumulation of DNA damage, attention has been focused on the possible role of specialised structures known as telomeres. These stretches of DNA, which can be up to hundreds of thousands of molecular units long, are situated at the end of each chromosome; a single human’s genetic code is packed into 23 pairs of chromosomes.
The significance of telomeres lies with the events that occur every time a cell divides. At each division the chromosomes must be duplicated to ensure that each of the daughter cells receives a complete set. Each time duplication occurs, a small part of the DNA at the end of each chromosome is lost, so the telomeres gradually shrink. After a certain number of cell divisions, the telomeres reach a critical length and the cell enters a non-dividing state. Upon any attempt to divide beyond this limit, the cell will undergo apoptosis (the ability of cells to self-destruct when something has gone wrong).
The link between telomeres and ageing originated from the discovery that increasing the levels of an enzyme capable of extending telomere length (telomerase reverse transcriptase or TERT) in mice brought about an increase in their life expectancy. Removing both copies of the gene that encodes for the TERT enzyme in mice coincided with shortened lifespan, increased frailty and reduced organ function.
Intriguingly, recent findings have indicated that some of the disparate theories of ageing are intimately linked. Mice lacking the TERT enzyme were shown to have impaired mitochondrial function and increased incidence of age-related disorders. It was discovered that the ill effects were mediated by p53. Many of the anti-cancer strategies utilised by cells depend on p53 and telomere shortening-induced cell death. There is growing evidence to suggest that the presence of these in-built anti-cancer mechanisms may be partly responsible for the ageing of stem cells.
We are still a long way from understanding the fine details of ageing, let alone its fundamental causes. Research has uncovered only some of the connections between the many answers to the question of why we age. It is likely that many more will be discovered. One thing is for sure: with ever increasing life expectancies in the developed world, an understanding of this seemingly inevitable process is becoming ever more important.
Andrew Szopa-Comley is a a 3rd year undergraduate in the Department of Zoology