MONDAY, 8 NOVEMBER 2010
It has a diameter of only 30 nanometres and you don’t even notice as it travels quietly through your gut and into your bloodstream. Poliovirus then infects your central nervous system and slowly destroys your neurons. Your muscles weaken rapidly and you will be paralysed for the rest of your life.Or would you rather choose the following scenario? When the needle pricks your skin you try to avoid looking. It hurts and you can feel the nurse press the liquid slowly into your tissue. Afterwards, your arm feels slightly numb where the injection was made, but you know that this short moment of discomfort will give you lifelong protection against polio.
 Every day, disease-causing pathogens attack people all over the world; the human immune system is constantly challenged by viruses and bacteria. Today, vaccinations are available for a wide range of diseases, and most people take them for granted. But this hasn’t always been true. Vaccination is probably the greatest medical invention in human history.
Every day, disease-causing pathogens attack people all over the world; the human immune system is constantly challenged by viruses and bacteria. Today, vaccinations are available for a wide range of diseases, and most people take them for granted. But this hasn’t always been true. Vaccination is probably the greatest medical invention in human history.Vaccine development began about 3000 years ago, when smallpox, a disease caused by variola virus, started to terrorise mankind. With a mortality rate of 30 per cent, smallpox was a serious threat to survival. The symptoms include fever, skin lesions and blindness, and there has never been an effective treatment. However, people began to look for a cure long before any of the cellular or molecular mechanisms were known.
Early on, it was discovered that people who survived a smallpox infection were immune to the disease for the rest of their lives. First described in 1022BC, a procedure called ‘variolation’ was developed, which protected against smallpox: material from a dried pustule of a person that survived smallpox was deliberately introduced into the skin or nose of a healthy person. This usually led to a mild infection followed by complete immunity to the virus. The procedure was not perfect however, two to three per cent of all those variolated did not survive the treatment. Diseases like syphilis and tuberculosis were also routinely transferred to patients. Health and safety regulations as we know them today would almost certainly not approve such a procedure, but at the time it saved the lives of many.
In the late 1700s, variolation was used regularly in China, India and Turkey. And so it came to the attention of Lady Mary Wortley Montagu, the wife of the British Ambassador to Turkey, who then introduced the method to England. During that time, people were desperate for help; smallpox was killing around 400,000 people each year in Europe. Variolation spread to the New World by 1721, and it became general practice to variolate soldiers before new military operations.
In 1757, the orphan child Edward Jenner was variolated in England. Jenner had always shown a great interest in medicine and biology. Not only did he study cuckoo hatchlings and their behaviour, he also carefully observed the people surrounding him. In doing so, he discovered that milkmaids who became infected with cowpox, from touching the udders of infected cows, would never develop the symptoms of smallpox. Although at that time it was not known that cowpox is caused by a virus that is closely related to variola virus, Jenner concluded that cowpox infection resulted in immunity to smallpox. To prove this, he used matter from a fresh cowpox lesion to intentionally infect an eight-year-old boy, who subsequently developed slight symptoms. Two months later he treated the boy with matter from a smallpox lesion. The boy didn’t develop any symptoms, and Jenner concluded that he was immune to smallpox. From the Latin word for cow, vacca, Jenner named his procedure ‘vaccination’ and published his results in 1798.
Despite biology textbooks stating that Jenner was the first person to carry out a vaccination, he had in fact been beaten to it. More than 20 years earlier, in 1774, the English farmer Benjamin Jesty carried out the same experiment. Jesty and at least five others who made the same discovery never published their results, so Jenner was given full credit for the first vaccination against smallpox. After its success was proven, vaccination spread quickly amongst European countries. Variolation was banned in the UK in 1842, and compulsory vaccination against smallpox was introduced in 1853.
After intensive vaccination programmes were established by the World Health Organisation in the 20th century, the number of smallpox infections declined rapidly. By 1979, smallpox had been successfully eradicated, demonstrating just how powerful vaccination can be – especially in the case of diseases that are transmitted exclusively by human hosts.
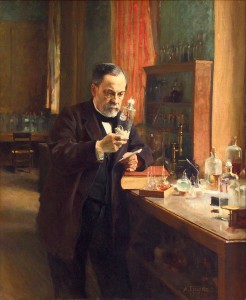
Many other scientists were able to build on the achievements of Jenner and his colleagues to further develop vaccination and immunology. One of these was Louis Pasteur, a French chemist and microbiologist. While he was studying the reasons for beer and milk going sour, he developed the idea that microorganisms could also cause disease in humans and animals. In 1880, coincidence helped him to understand one of the fundamentals of vaccination. He was working on chicken cholera, a fatal disease transmitted by bacteria. When some of his chickens were infected with an old culture of bacteria, they only developed minor symptoms and recovered fully. Pasteur suspected that these chickens would now be immune to chicken cholera; he was right. After infecting them with a fresh culture of bacteria, the pre-immunised chickens did not develop any symptoms.
Pasteur had proven that artificially weakened pathogens could be used as vaccines. He applied the same principle to generate a rabies treatment in 1884. Pasteur expanded the definition of a vaccine to include all administered solutions that contain attenuated or inactivated pathogens (or parts of them) that induce immunity in the vaccinated individual.
In the following century, the improvement and development of new vaccines was mainly shaped by one person: the American microbiologist Maurice Hillemann. Unknown to many people, he developed more than 40 vaccines during his career, including vaccines against measles, mumps, Hepatitis A and B, chickenpox, rubella and pandemic flu. His achievements are estimated to save the lives of nearly eight million people each year. Fourteen of his vaccines are still part of current vaccine schedules. Hillemann’s ability to decimate pathogens was unrivalled. When his five-year-old daughter Jeryl Lynn fell ill with mumps, he used the opportunity to combat the virus. By collecting samples from her, he was able to culture the virus in the cells of chicken embryos. From there, he proceeded to make an attenuated form of the virus – which served as the world’s first live vaccine against mumps – still known as the Jeryl Lynn strain. Hillemann also produced the well-known MMR vaccine, which combines three attenuated viruses and gives protection against measles, mumps and rubella.
The examples of Jenner, Pasteur and Hillemann show that coincidences and observations outside of the lab played a critical role in the history of vaccine development. Today, the UK immunisation schedule encompasses vaccines against 11 diseases. However, vaccine development is not without challenges or controversy. There are many diseases for which researchers have not succeeded in developing an effective vaccine. Two of the most devastating are HIV and malaria, which together cause three to five million fatalities each year. Criticism from the general public is also common; the necessity and side effects of vaccinations are commonly debated. Like any other drug or medication, vaccination can have side effects. But if we consider how many people have been saved from lifelong illness and death, and if we think of diseases like smallpox (which was successfully eradicated) or polio (which is close to being eradicated), vaccination can surely be considered the greatest medical discovery ever made.
Stephanie Glaser is a PhD student in the Department of Biochemistry